Blood cancers impact the formation and functioning of your child’s blood cells. While regular blood cells will reproduce and die, cancerous blood cells do not die and instead continuously reproduce and push out the healthy blood cells. The two most common types of hematologic cancers in children are leukemia and lymphoma. Acute Lymphoblastic Leukemia (ALL) — more commonly called blood cancer is the most prevalent.
A diagnosis of blood cancer in a child can be emotionally overwhelming for parents. It’s natural to feel confused by the medical terms and the treatment plans. However, understanding what’s happening can help parents feel more in control and give them the strength needed during the treatment journey.
What is Leukemia?
The word “Leukemia” comes from the Greek words leucos (white) and haima (blood), meaning an excess of white blood cells. In simple terms, leukemia is cancer of the white blood cells.
Role of the Bone Marrow
The bone marrow is the soft, spongy tissue inside our bones. It makes three important types of blood cells:
- White blood cells (WBCs): Help fight infection.
- Red blood cells (RBCs): Carry oxygen through hemoglobin.
- Platelets: Help in blood clotting ,thereby prevent excess bleeding.
In blood cancer, the bone marrow starts producing abnormal white blood cells in large numbers, called blasts. These immature cells crowd out the healthy blood cells, just like weeds in a garden, stopping flowers from growing. As a result, children may develop:
- Anemia (low RBCs)
- Neutropenia (low WBCs)
- Thrombocytopenia (low platelets)
Causes of Blood Cancer in Children
Most parents wonder what caused their child’s illness. However, in most cases, there is no known reason. Some rare cases may be linked to genetic conditions like Down syndrome. While exposure to radiation and chemicals like pesticides has been studied, no direct cause has been confirmed. It’s important to note that blood cancer is not contagious and cannot spread from one child to another.
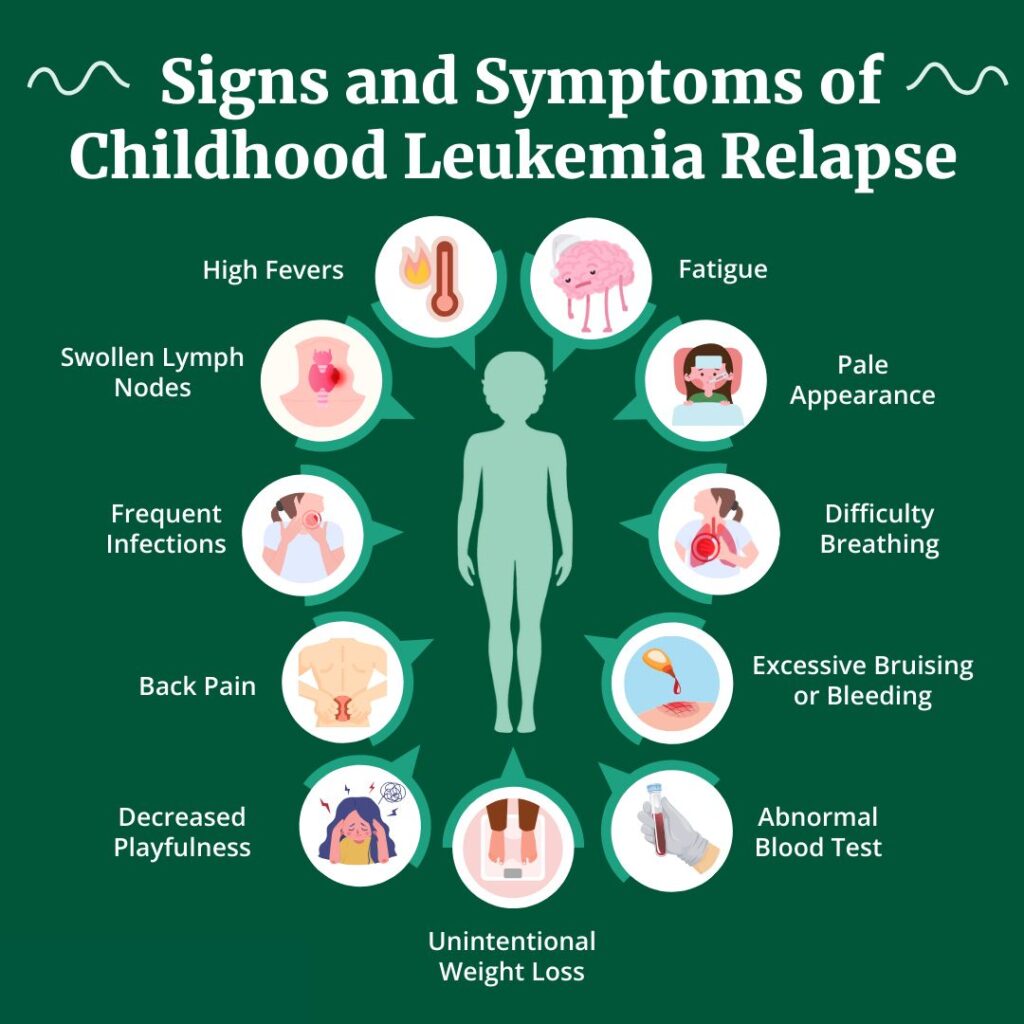
Common Symptoms, which Children with blood cancer may present, are:
- Frequent fevers and infections
- Pale skin and tiredness
- Unusual bruising or bleeding (especially from the gums or in areas without injury)
- Swollen lymph nodes
- Bone or joint pain
- Difficulty in walking or refusal to bear weight in younger children
However, many of these symptoms are common in kids and don’t always mean cancer. Still, if these symptoms persist, consult a doctor.
Diagnosis of hematologic cancers
The first test is usually a complete blood count (CBC). It checks the levels of blood cells and may show abnormal white cells. However, sometimes the CBC may appear normal. To confirm leukemia, doctors would do a bone marrow test, which involves collecting a small sample of marrow, usually from the hip bone. This is done under sedation or anesthesia and causes only temporary discomfort.
Other tests include:
- Flow cytometry and cytogenetics: To classify the cancer type
- Lumbar puncture: To check if cancer cells have reached the fluid around the brain and spine (CSF)
Treatment for hematologic cancers in children
Treatment usually begins with the treatment of early symptoms such as anemia (low red blood cells), bleeding, or infections. Then, a combination of treatments can be employed based on the child’s condition:
Chemotherapy: These are drugs taken orally or by IV (into a vein). They target rapidly growing cells such as cancer cells. They can also target healthy cells, causing side effects.
Intrathecal chemotherapy: Drugs are directly injected into the space surrounding the spinal cord to treat cancer cells in the brain and spinal fluid.
Radiation therapy: Special energy beams, such as X-rays, are directed to kill cancer cells. This can also relieve pain due to inflamed organs or bone marrow pressure.
Stem cell or bone marrow transplant: Intensive chemotherapy (and, at times, radiation) is first administered to destroy the cancer cells in the bone marrow. Healthy stem cells from a donor are then infused through an IV. These cells migrate to the bone marrow and begin producing healthy blood cells again.
Immunotherapy (Biological therapy): Specific antibodies are employed to enable the immune system to identify and kill cancer cells. Some also aid in the delivery of medicine straight to the cancerous tissue.
Supportive medicines: Medications can be administered to control side effects like nausea, pain, or to guard healthy cells during treatment.
Blood transfusions: Employed to replace shed red blood cells or platelets.
Antibiotics: These are administered to prevent or cure infections during therapy when the immune system is compromised.
Follow-up care: Checkups are essential to monitor how well the treatment is progressing, detect if the cancer comes back, and observe for any late side effects.
Is a Bone Marrow Transplant Always Needed?
Not always. Most children with ALL respond well to chemotherapy alone. A bone marrow transplant is considered only in cases where the child doesn’t respond well to chemo or has high-risk features in their test reports.
New Challenges and Support Systems in India
In India, childhood blood cancer care is improving, but families still face many challenges. These include:
- Delayed diagnosis due to lack of awareness
- Financial stress, as treatments can be long and costly
- Limited access to pediatric cancer centers, especially in rural areas
However, the good news is that support systems are growing:
- Many government hospitals now offer free or subsidized treatment.
- NGOs and foundations are helping families with financial aid, accommodation, and counselling.
- Awareness programs in schools and communities are helping with early detection.
- Pediatric oncology units are being developed in major cities, providing specialized care.
Being informed and seeking support early can make a big difference in the outcome and overall experience for both the child and their family.
FAQ’s for Hematologic Cancers in Children: Types, Causes, Symptoms, Diagnosis, Treatment and Support Challenges in India
Hematologic cancers are cancers that begin in the blood-forming tissue, such as the bone marrow or lymphatic system. In children, the most common types are leukemia and lymphoma.
The exact cause is often unknown. However, rare cases may be linked to genetic disorders like Down syndrome or exposure to radiation or chemicals. Blood cancer is not contagious.
Common signs include:
Frequent infections or fevers
Pale skin and tiredness
Unexplained bruising or bleeding
Swollen lymph nodes
Bone or joint pain
Diagnosis usually starts with a Complete Blood Count (CBC). Confirmation is done through a bone marrow aspiration/ biopsy and additional tests like flow cytometry and lumbar puncture.
Yes, Acute Lymphoblastic Leukemia (ALL) in children is highly treatable. With early diagnosis and the right treatment, survival rates have improved significantly to around 80-85%.
Treatment may include:
Chemotherapy
Radiation therapy
Intrathecal chemotherapy
Stem cell or bone marrow transplant
Immunotherapy
Supportive medications and blood transfusions
No. Most children with ALL respond well to chemotherapy. A bone marrow transplant is only considered in high-risk or relapsed cases.
Key challenges include:
Delayed diagnosis
High treatment costs
Limited pediatric oncology centers, especially in rural areas
Support includes:
Free or subsidized care in government hospitals
NGO support for accommodation and finances
Counselling services
Increasing number of specialized pediatric oncology units
Regular follow-up helps:
Track recovery
Detect relapse early
Manage long-term side effects of treatment.
Ensure near normal growth and development of the child.
Author: Dr. Srikanth Marda
Consultant Pediatric Oncologist and Hematologist